Glaucoma Treatment
Dedicated glaucoma care to ensure
your eyes stay healthy and vision stays clear

What is Glaucoma?
Glaucoma is a condition where the pressure inside the eye increases, damaging the optic nerve. This damage can lead to gradual, permanent visual field loss if not treated early. Often called the “silent thief of sight,” glaucoma usually shows no symptoms until it has already affected vision. Regular eye check-ups are the best way to catch it early and prevent long-term damage.
Symptoms You May Notice
- Gradual loss of side (peripheral) vision
- Blurred or tunnel vision
- Eye pain or pressure
- Redness in the eye
- Seeing halos around lights
- Headaches or nausea (in acute cases)
- Difficulty seeing in low light
When to See a Doctor?
Since glaucoma often develops without warning signs, routine eye exams, especially after age 40, are crucial. If you have a family history of glaucoma or notice any changes in your vision or eye pressure, consult an eye specialist right away. Early detection can help manage the condition and prevent vision loss.
Need help with your eyes?
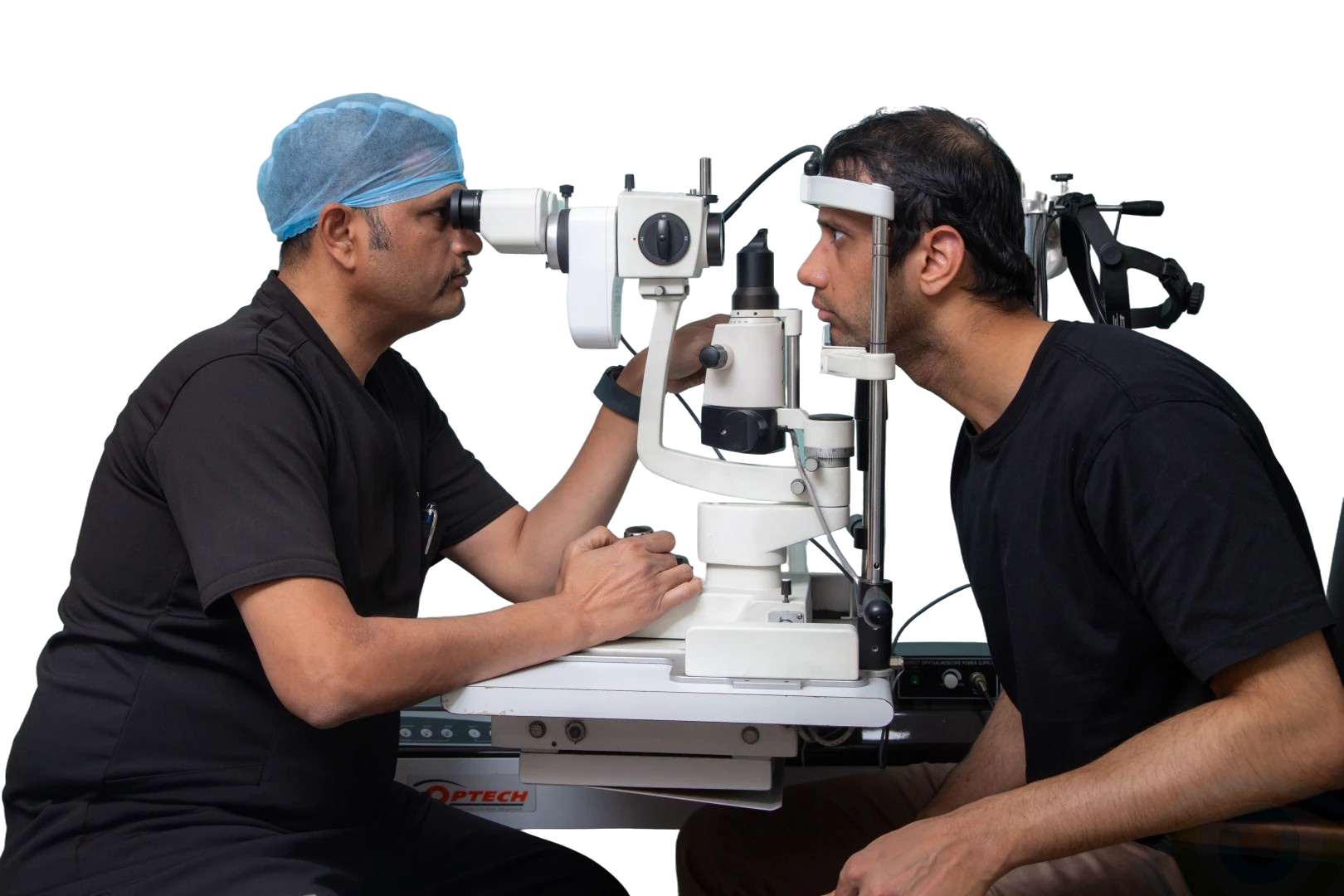
Our Treatment Approach
- We focus on early detection and long-term management of glaucoma to prevent vision loss.
- Our glaucoma evaluation involves a detailed eye pressure check, gonioscopy, pachymetry, perimetry (visual field test), and Optical Coherence Tomography (OCT) of the optic nerve. These tests help us understand the type and extent of glaucoma.
- Based on this information, we develop a tailored treatment plan that may include medicated eye drops, laser procedures, or surgery to control intraocular pressure and protect your vision.
Chosen by Patients.
Trusted for Outcomes.
- Early detection using advanced diagnostics like OCT and perimetry
- Expertise in managing all types of glaucoma: open-angle, angle-closure, and secondary glaucoma
- Medical, laser, and surgical options
- Patient-friendly guidance for lifelong glaucoma management
- Consistent monitoring to maintain existing vision
- Trusted by patients for compassionate, precise care

FAQs
Can glaucoma lead to total blindness?
Yes, glaucoma causes a gradual loss of peripheral (side) vision. If left untreated, it can progress to complete blindness. In acute cases, vision loss can happen quickly and become permanent if not addressed immediately.
What causes glaucoma?
Glaucoma happens when the optic nerve, which connects your eye to your brain, gets damaged. This damage usually comes from increased pressure in the eye due to fluid buildup (aqueous humor) that doesn’t drain correctly.
Why does eye pressure increase and damage the optic nerve?
Normally, fluid in the eye drains through a mesh-like system where the iris meets the cornea. If this drainage slows down or gets blocked, fluid builds up inside the eye. This raises the intraocular pressure (IOP), damaging the optic nerve.
Other less common causes include:
- Eye injuries (chemical or blunt trauma)
- Eye infections
- Inflammatory eye diseases
- Complications from eye surgery
What are the types of glaucoma?
Open-Angle Glaucoma (most common):
- Drainage slows over time
- No early symptoms or pain
- Gradual loss of peripheral vision
- Can progress unnoticed without regular eye exams
Closed-Angle (Narrow-Angle) Glaucoma:
- The iris blocks the drainage angle
- Can cause a sudden increase in pressure (acute attack)
- Requires emergency treatment
- Signs of an acute attack include:
- Sudden blurry vision
- Severe eye pain
- Headache, nausea, vomiting
- Halos or rainbow rings around lights
If you have diabetes or a systemic history of diabetes or hypertension, you may be at risk of developing chronic closed-angle glaucoma, where the blockage builds up over time.
Who should get tested for glaucoma?
- If you have a family history, get tested once a year.
- If there’s no history and you’re under 40, test every 5 years.
- Over 40? Test every 2 to 3 years.
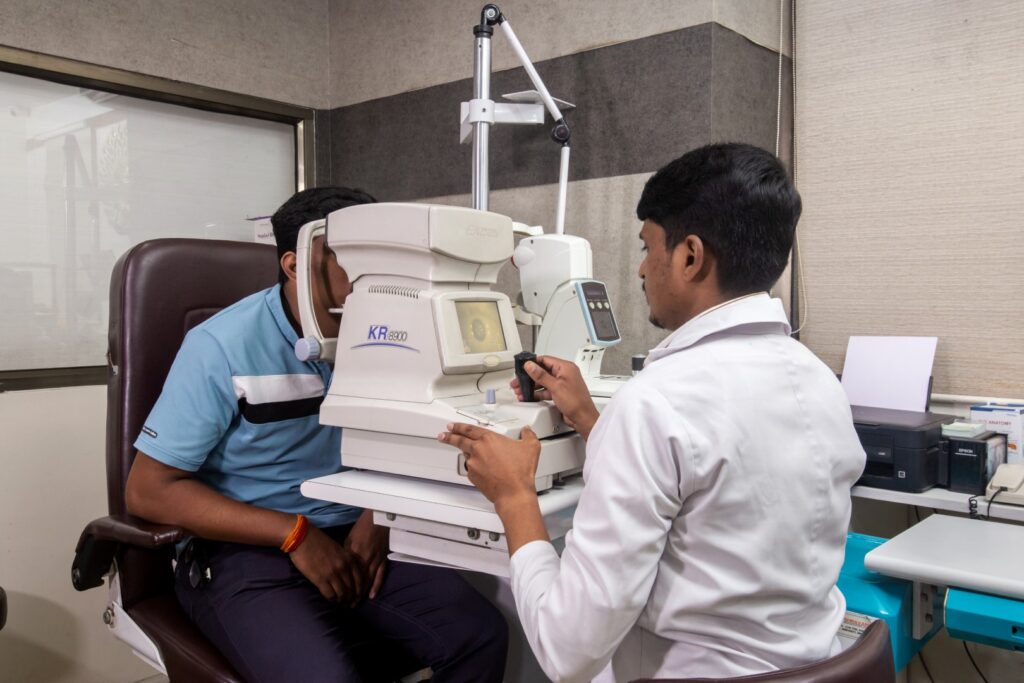
How is glaucoma diagnosed?
- Ophthalmoscopy: Examining the optic nerve
- Perimetry: Testing your visual field
- Gonioscopy: Checking the angle between the iris and cornea
- Pachymetry: Measuring corneal thickness
- OCT (Optical Coherence Tomography): Imaging the optic nerve
How is glaucoma treated?
Treatment aims to lower eye pressure to prevent damage. Options include:
Eye Drops: First line of treatment; must be used consistently.
Oral Medication: Used if drops aren’t effective. May have side effects.
Laser Treatment: For open-angle glaucoma: Improves fluid drainage.
- For closed-angle glaucoma: Creates a new drainage pathway.
- Quick procedure, usually allows you to resume daily activities the next day.
Traditional Surgery (Trabeculectomy):
- Creates a new drainage path.
- Often reduces or removes the need for medication.
- Recovery takes about 4 to 8 weeks.
Tube Shunt Surgery:
- A silicone or polypropylene tube is implanted.
- Redirects fluid to a reservoir for absorption.
- Often used when other treatments fail.
- Ahmed Glaucoma Valve is a commonly used type.
Cycloablation (Cyclophotocoagulation):
- Destroys part of the fluid-producing tissue with a laser.
- Used as a last option when other surgeries don’t work.
Are there any risks with glaucoma surgery?
All surgeries have some risks:
Laser Risks:
- Temporary spike or drop in eye pressure
- Slight risk of cataract development
Incisional & Shunt Risks:
- Leaks, infections (blebitis, endophthalmitis)
- Low pressure (hypotony), retinal or choroidal detachment
- Corneal damage, double vision, cataract formation
- Shunts may need to be replaced eventually
Your doctor will discuss the best option based on your condition and overall health.